Pediatric Sleep Disorders:
Information and Resources
Sleep disorders not only affect adults. They also affect infants, children, and adolescents. Children that suffer from poor sleep also tend to have other problems. These include developmental, behavioral, social, health and academic challenges. Pediatric sleep disorders not only impact a child’s health. They also affect the family interactions, as well as the sleep of parents and siblings.
Such sleep disorders are characterized by:
- Difficulties falling or staying asleep
- Obstructive sleep apnea
- Sleepwalking
- Restless movements all night
- Excessive sleepiness during the day
- Cataplexy
These symptoms that present in children are not the same as those of adults with the condition.

Diagnosing Pediatric Sleep Disorders
Medical professionals will conduct a complete history and physical exam to assess each child’s symptoms. The information that is normally collected about each child focuses on the:
- Home environment
- Sleeping environment
- Medical history
- Prior sleep history and testing
- School performance (if applicable)
- Parents’ sleep quality
To further aid diagnosis, the child may need to stay overnight for a sleep study. Some blood tests may be done as well. The physician may also request that the parents keep a sleep diary of the child’s sleep patterns as well.
Medical Disorders That May Lead to Sleep Disorders
There are several underlying conditions that may result in sleep disorders. They include:
Arousal Disorders
In this case, the child doesn’t fully awake from sleep, as this is partial arousal or slow-wave sleep. When children awake in this stage, they may be in a confused state as they are between sleeping and waking. Sometimes the child may cry loudly, move or even run. In spite of this, they remain disoriented and unresponsive to any stirring attempts.
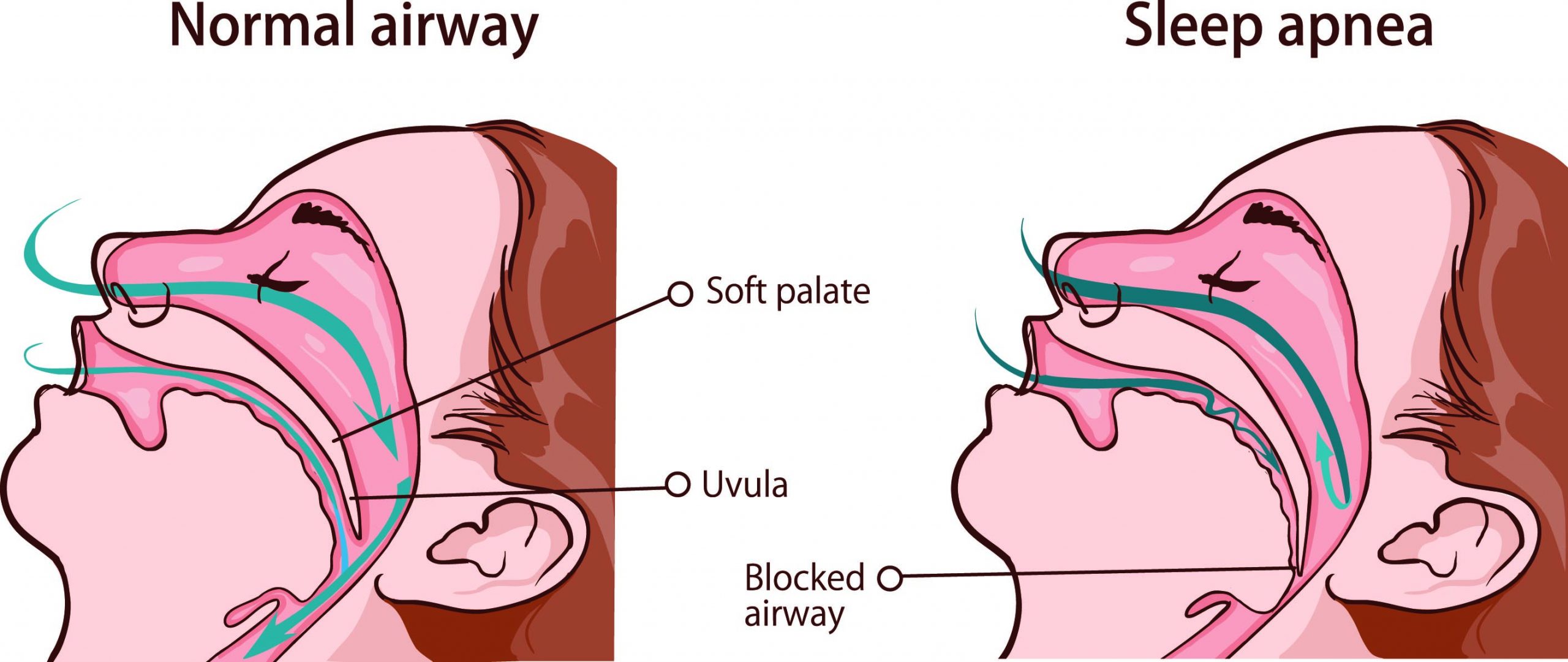
Snoring
Snoring occurs when the airway is partially blocked and inhalation is restricted. This excess air is redirected to the mouth. It vibrates the soft tissue in the palate. This then creates the snoring sounds. This snoring disrupts sleep which makes a child fatigued and sleepy during the day.
Diagnosing Pediatric Sleep Disorders
Medical professionals will conduct a complete history and physical exam to assess each child’s symptoms. The information that is normally collected about each child focuses on the:
- Home environment
- Sleeping environment
- Medical history
- Prior sleep history and testing
- School performance (if applicable)
- Parents’ sleep quality
To further aid diagnosis, the child may need to stay overnight for a sleep study. Some blood tests may be done as well. The physician may also request that the parents keep a sleep diary of the child’s sleep patterns as well.
Medical Disorders That May Lead to Sleep Disorders
There are several underlying conditions that may result in sleep disorders. They include:
Arousal Disorders
In this case, the child doesn’t fully awake from sleep, as this is partial arousal or slow-wave sleep. When children awake in this stage, they may be in a confused state as they are between sleeping and waking. Sometimes the child may cry loudly, move or even run. In spite of this, they remain disoriented and unresponsive to any stirring attempts.
Snoring
Snoring occurs when the airway is partially blocked and inhalation is restricted. This excess air is redirected to the mouth. It vibrates the soft tissue in the palate. This then creates the snoring sounds. This snoring disrupts sleep which makes a child fatigued and sleepy during the day.

Obstructive Sleep Apnea (OSA)
OSA occurs when the airway is completely obstructed or partially collapses during sleep. This can even cause the throat’s soft tissue to relax. As a result, it can block the upper airway enough to disrupt normal breathing patterns. This may then cause the child to suddenly awake in order to breathe normally. Often, the child then falls asleep. So an entire night may pass in a cycle of abrupt awakenings and drifting off to sleep
Upper Airway Resistance Syndrome (UARS)
UARS is like OSA in that the soft tissue in the throat relaxes, and restricts the passage of air into the lungs. The increased blockage in the upper airway is not as extensive as OSA. But it does cause a brief awakening from sleep that’s often undetected. Many repeated episodes of these awakenings can disrupt sleep.
Central Sleep Apnea (CSA)
CSA and sleep-related hypoventilation/hypoxemic syndromes affect respiratory conditions. In this case, CSA arises when the brain doesn’t cue the body to breathe during sleep. This is different from OSA and UARS, as there is no breathing to obstruct. CSA is characterized by episodes of shallow breathing. These episodes last for more than 10 seconds during sleep.

Restless Legs Syndrome (RLS)
RLS and periodic limb movements during sleep (PLMS) are two distinct sleep disorders. RLS is neurological in its cause and has a severe impact on a child’s health and quality of life. However, PLMS has no known cause. These increased movements during sleep may lead to fatigue, depression and heart conditions.
Insomnia
Does your child resist going to bed every evening, trying to fight sleep? Insomnia manifests with distinct night- and day-time symptoms. Night-time symptoms mean problems falling and/or staying asleep, or having non-restorative sleep. Day-time symptoms involve:
- A reduced sense of wholeness
- Problems in completing daily tasks
- Loss of concentration
- Compromised memory
- Fatigue
An insomnia diagnosis is likely when the symptoms last from 1 to 6 months.
Parasomnias (or Nighttime Sleep Behaviors)
These are sleep disorders that involve unusual behaviors at night. These parasomnias can occur at any time. Some of these abnormal behaviors include:
- Sleepwalking or sleep talking (but the child is still unconscious or asleep)
- Sleep terrors (a sense of extreme fear and a temporary inability to wake up)
- Confusional arousals (the child seems to be awake but is still asleep )
- REM behavior (the child physically acts out his/her dreams)
- Sleep paralysis
- Nightmares
Restless Legs Syndrome (RLS)
RLS and periodic limb movements during sleep (PLMS) are two distinct sleep disorders. RLS is neurological in its cause and has a severe impact on a child’s health and quality of life. However, PLMS has no known cause. These increased movements during sleep may lead to fatigue, depression and heart conditions.
Insomnia
Does your child resist going to bed every evening, trying to fight sleep? Insomnia manifests with distinct night- and day-time symptoms. Night-time symptoms mean problems falling and/or staying asleep, or having non-restorative sleep. Day-time symptoms involve:
- A reduced sense of wholeness
- Problems in completing daily tasks
- Loss of concentration
- Compromised memory
- Fatigue
An insomnia diagnosis is likely when the symptoms last from 1 to 6 months.
Parasomnias (or Nighttime Sleep Behaviors)
These are sleep disorders that involve unusual behaviors at night. These parasomnias can occur at any time. Some of these abnormal behaviors include:
- Sleepwalking or sleep talking (but the child is still unconscious or asleep)
- Sleep terrors (a sense of extreme fear and a temporary inability to wake up)
- Confusional arousals (the child seems to be awake but is still asleep )
- REM behavior (the child physically acts out his/her dreams)
- Sleep paralysis
- Nightmares

Treating Pediatric Sleep Disorders
Treatment of pediatric sleep disorders begins with establishing expectations about what constitutes regular pediatric sleep. Implementing behavior modification plans may resolve some sleep problems. These plans may include:
- Scheduled waking
- Positive reinforcement
Physicians may also prescribe medications for specific sleep disorders or their underlying conditions.
In some instances, resolving sleep disorders may require an ENT (Ear, Nose and Throat) specialist. Other interventions may require:
- Surgery
- Orthodontics
- Sleep apnea mask – to maintain continuous positive airway pressure


![]()
Pediatric Sleep Disorders Prognosis
Children need adequate sleep to grow and meet their developmental milestones. So any disruptions to their sleep are likely to hurt their wellbeing. These sleep disorders may also continue into adolescence if they are not resolved.
![]()
Pediatric Sleep Disorders Prognosis
Children need adequate sleep to grow and meet their developmental milestones. So any disruptions to their sleep are likely to hurt their wellbeing. These sleep disorders may also continue into adolescence if they are not resolved.

Accessing Healthcare
for Pediatric Sleep Disorders
If your child is displaying symptoms of pediatric sleep disorders or the underlying conditions, then please arrange an initial consultation with us. Our team of experts at Family Neurology will be able to assess your child. We will also be able to render the appropriate healthcare. We will work with you, your child and your family to create the appropriate treatment plan.


Pediatric Sleep Disorders Resources
Websites
The following websites present useful information about pediatric sleep disorders:
Pediatric Sleep Disorders Resources
Websites
The following websites present useful information about pediatric sleep disorders:

Call Us to Make an Appointment
Phone: 713-589-7020
Fax: 713-999-9095
3301 Plainview St, Suite 8
Pasadena, Texas 77504